Aging and Dental Health
With the improvements of healthcare measures, life expectancy is increased. It is normal for a person to live up to 80, 90. Longer life goes along with the higher oral health issues. However, good oral care and effective prevention can render a healthy mouth. As you age, your mouth may have those changes:
Gum recession:
There are many factors that cause gum recession: applying too much pressure when you brush your teeth; insufficient dental care or smoking that cause plaque and calculus accumulation, calculus trigger gum recession; untreated gum disease also causes this problem… Once the gum margin is receded, root surface would be exposed. Root surface have no enamel protection and prone to sensitive to hot or cold. Root surface has higher risk of caries. Dimension of the root is smaller than the coronal part of the teeth, receded gum would leave larger spaces between the teeth, those spaces tend to trap food, which cause gum discomfort and root caries.

Root caries:
Root caries are prevalence in elderly individuals. The risk of root caries in this group is 3 times higher than the young people. More than 60% of people above 65 years old have root caries. Root caries is fast spreading to the pulp than cavity of the chewing surface because the thickness of dentin in the root is much smaller.

Root caries detection is tougher if the cavity locates below the gum surface; X ray images may help to detect root caries.
The retention of fillings on the root cavity are even tougher because the bonding of the filling materials on the root dentin is weaker compare to the bonding on the enamel of the chewing surfaces.
Prevention of root caries includes stricter oral hygiene, limit snack times during the day and application of fluoride to increase the resistance of dentin to caries process.
Tooth wear:
Tooth structure can withstand the abrasion to help you masticating foods. However, when you have poor oral habit as bruxism or clenching your teeth, the signs of tooth wear will be obvious.

Once enamel layers have worn down, softer underlying dentine will be worn at a faster speed. Severe tooth wear may end up with shortening of tooth to the gum surface. Porcelain crowns and bridges made of harder materials than enamel is also a contributing factor to severe tooth wear.
Wearing night guard is one way to slow down tooth wear, especially when you are bruxer or clencher.
Gum disease:
Gum disease is prevalent in elderly people. The commonness of the disease may be up to 70% of the aged population. Tissues around the teeth can be damaged by the toxins of bacteria that cause gum disease. Damaged bone cells and ligaments around the teeth would die and lost; the teeth become mobile, oozing pus at the gum and end up with tooth lost.
The prevention and treatment of gum disease will be discussed in depth in the related topics.

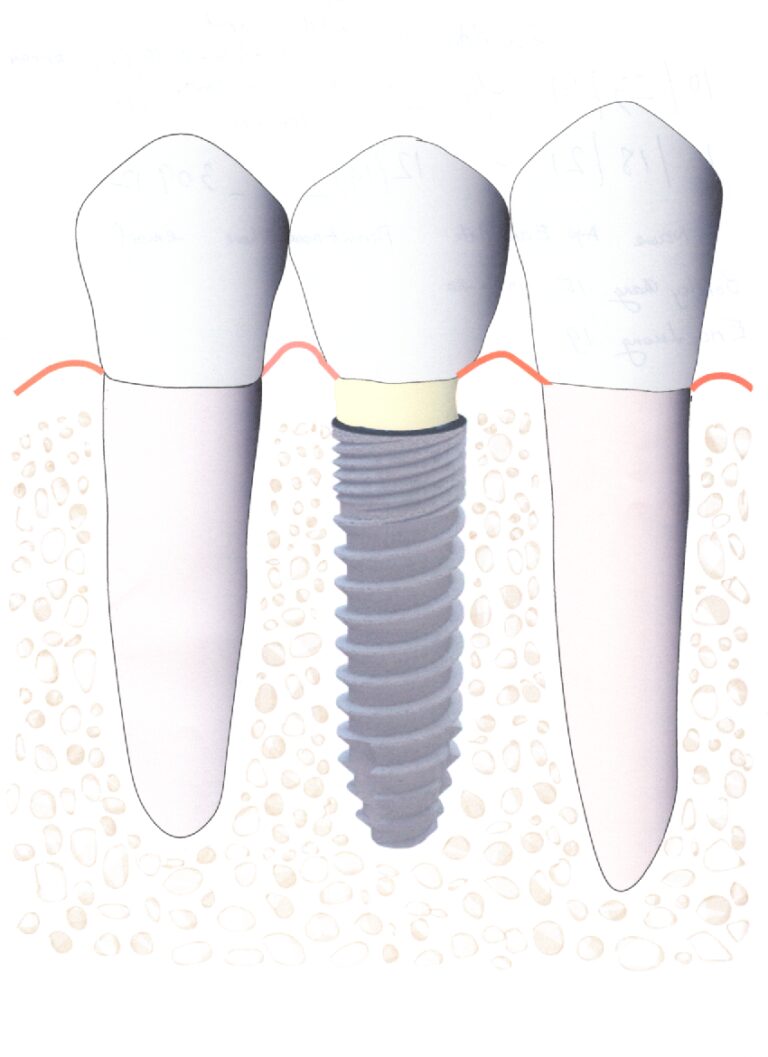
Missing teeth:
Missing teeth is common in aged population. There is only 2% of people above 65 years old who still have full dentition. Most of missing teeth are caused by caries and gum disease. Therefore, missing teeth can be prevented by controlling those two diseases since the childhood.
Once one tooth is missing, it should be replaced by an artificial tooth (we call it prosthesis) or an implant to prevent the shifting of the remaining teeth. One missing molar may reduce the chewing efficiency to 25%.

Dry mouth:
This is a reduction in production of saliva. Symptoms can range from mild to severe and include: a dry, sticky feeling in the mouth; saliva become thick or stringy; painful, burning sensation in the mouth or tongue; difficulty chewing, talking or swallowing. Dry mouth can be caused by diseases of the salivary glands, side effects of different medications, radiation therapy of the head and neck cancer.
Normal amount of saliva helps to lubricate and retain the full dentures in the oral cavity. Dry mouth poses difficulties in denture wearing: dentures cause pain and irritation of the oral mucosa; retention of denture is compromised.
More information about dry mouth is presented in the topic “Dry Mouth”.

Difficulties in oral care:
Patient with osteoarthritis, Parkinson, stroke may experience difficulties in oral care and this problem may lead to dental caries and gum disease. A good oral care is very important for elderly people, especially for the seniors who live in nursing homes. Electric toothbrush may be helpful for individuals with poor dexterity. Routine dental care should be maintained to ensure good oral health.
Nutrition:
Aging population have higher risk of missing teeth and reduction in chewing ability. This disadvantage leads to a shifting of diet to softer food like cake, soft candies. There is a change of tastes in aging with a tendency to consume more sugar; this may lead to higher risk of dental cavities.
To lower the risk of caries, the ideal diet should have:
- More fruits and vegetables, those foods have more vitamins and fibers. Those are good for nutrition, digestion and keep the teeth cleaned by the massage of food fibers to tooth surfaces.
- Reduction in consuming of carbohydrates especially sweet foods, sweet beverages.
- Limit snack time during the day and brushing teeth after every single meal.

Difficulties in denture wearing:
After many years of supporting denture, residual ridge of the jaw changes size and shape, therefore dentures become ill-fitted. Ill- fitted dentures tend to cause sore spots, discomfort. The impact of unstable denture would accelerate the resorption of the jaw bone.
Denture wearer should have regular dental checkup, denture base should be relined every year to make it fit.
Denture care is also a burden to the persons who cannot take care for themselves. Care givers should know how to provide oral care to patients and take care for patient’s dentures.
In summary, the prevention and treatment of dental problems pose a challenge to the elderly people and to the healthcare providers.
Good habits in oral care since the childhood would bring up a healthy mouth and well-being in the aging.